Typical Symptoms
Positive Symptoms
Additions to normal experiences:
- Hallucinations - Seeing, hearing, or feeling things that aren't there
- Delusions - False beliefs not based in reality
- Disorganized speech - Incoherent or illogical speech patterns
- Abnormal movements - Agitated or bizarre body movements
Negative Symptoms
Reductions in normal experiences:
- Flat affect - Reduced emotional expression
- Anhedonia - Inability to feel pleasure
- Avolition - Lack of motivation
- Social withdrawal - Isolation from others
- Alogia - Reduced speaking
Cognitive Symptoms
- Attention deficits
- Memory problems
- Executive function impairment
- Processing speed reduction
Facilitation Tip
Collect and categorize the patients' symptoms (for example on a flipchart). Explain that "plus symptoms" are additions to normal experience, while "minus symptoms" represent something less compared to normal energy/functioning levels.
Typical Course of Schizophrenia
Phases
- Prodromal Phase - Early warning signs including social withdrawal, decreased functioning, and unusual behaviors
- Acute Phase - Full manifestation of positive symptoms including hallucinations and delusions
- Stabilization Phase - Symptoms begin to resolve with treatment
- Maintenance Phase - Symptoms are controlled but require ongoing management
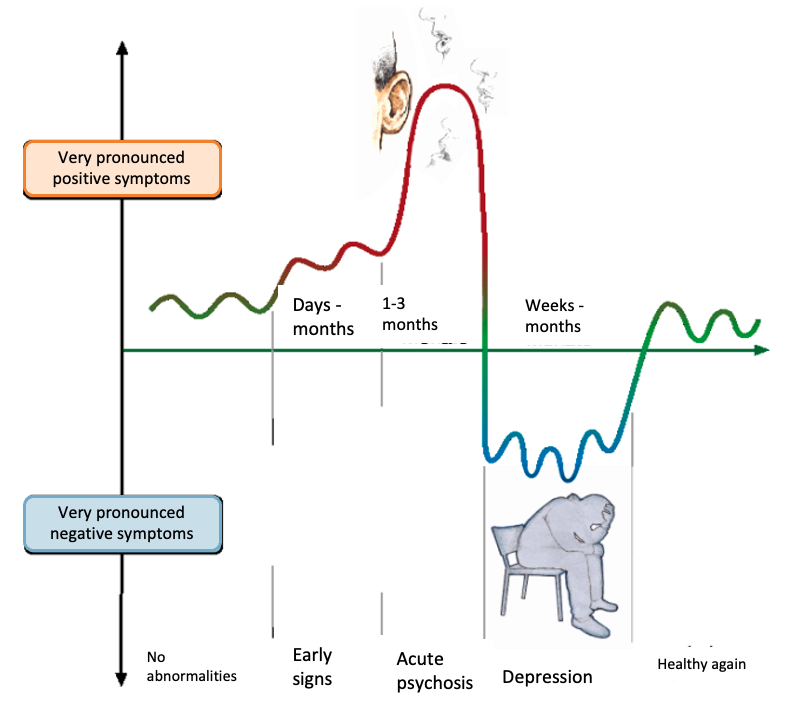
Visual representation of different course patterns in schizophrenia, showing symptom intensity over time
Course Patterns
- Single episode with full recovery (rare)
- Multiple episodes with partial or full recovery between episodes
- Multiple episodes with increasing disability
- Continuous symptoms with varying severity
Risk Factors for Worse Course
- Younger age at onset
- Longer duration of untreated psychosis
- Poor premorbid functioning
- Substance use
- Lack of social support
- Poor treatment adherence
The course of schizophrenia is not fixed and can be positively influenced by appropriate treatment and management strategies. With proper treatment and support, many patients can achieve stability and improvement over time.
Risk Factor: Cannabis
Cannabis use is associated with an increased risk of developing schizophrenia, particularly in vulnerable individuals.
Key Facts
- Cannabis use can increase the risk of psychosis by 2-4 times
- The risk is higher with more potent forms of cannabis (high THC content)
- Starting cannabis use at a younger age (adolescence) increases risk
- For people with schizophrenia, cannabis can:
- Trigger symptom relapses
- Reduce effectiveness of treatment
- Lead to poorer long-term outcomes
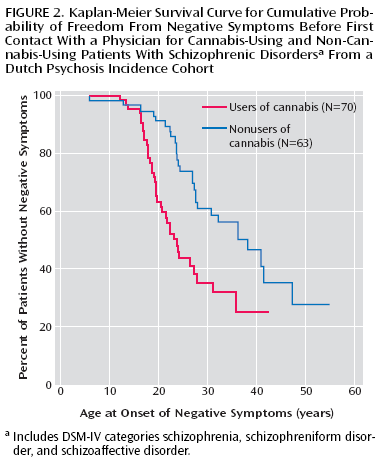
Cannabis and Brain Development
Important: Cannabis affects brain development during adolescence and can interact with genetic vulnerability to increase schizophrenia risk.